When it comes to women's reproductive health there is often a lot of talk about 'estrogen dominance', but what exactly does estrogen dominance mean? Get the facts on estrogen and progesterone, 'estrogen dominance' and hormonal imbalance.
What is Estrogen?
Although we think of estrogen as a female sex hormone, it is an important metabolic sex steroid hormone in both female and male bodies. In female bodies it's cyclical production causes the ripening of a follicle, growth of the endometrium and ovulation of a ripened egg. It also helps to regulate sexual desire, sleep (circadian rhythm), moods and energy levels.
To understand estrogen and the concept of estrogen dominance you really need to also understand progesterone and how both these female sex hormones change throughout your menstrual cycle.

How Does Estrogen Change Through the Menstrual Cycle?
Estrogen levels vary throughout the menstrual cycle. The menstrual cycle starts on day 1 of your period. Estrogen is at a baseline low level on day 2-3 of your cycle.
During the first half of a woman's cycle (or follicular phase), estrogen levels rise. Estrogen is produced by the ovary in response to FSH (follicle stimulating hormone) and rises until it reaches its peak around day 14, which is when ovulation occurs.
After ovulation ,the level of estrogen reduces from it's pre-ovulation peak, but remains fairly high until the end of the second half of the cycle (luteal phase) when it returns to baseline just before your next period.

How Does Progesterone Change Through the Menstrual Cycle?
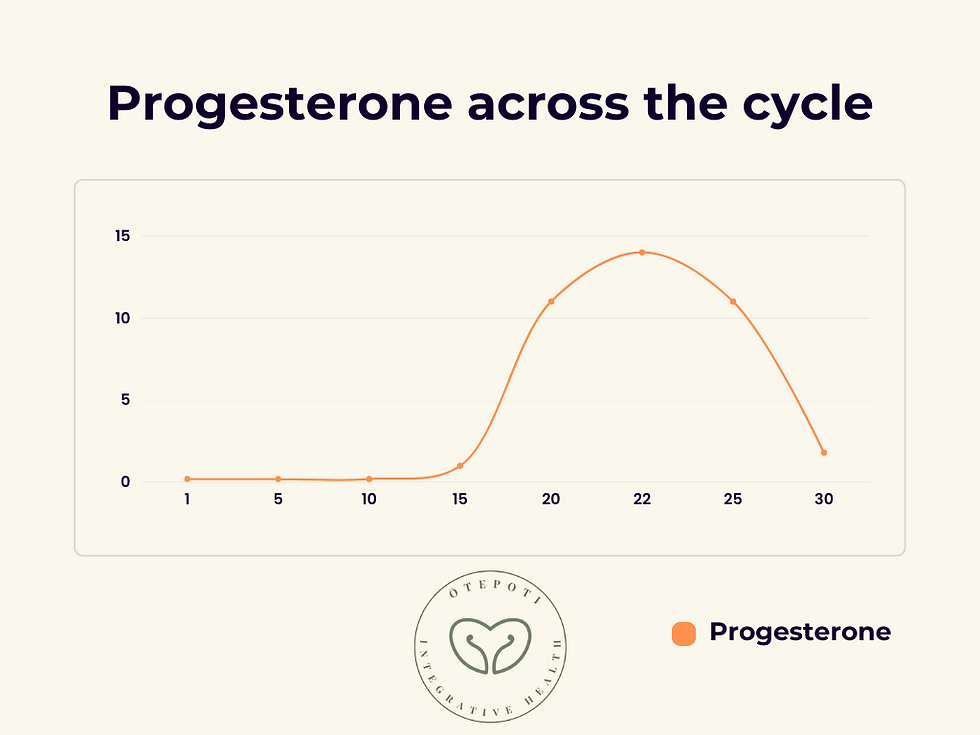
Progesterone is an important sex steroid hormone released during the luteal phase (second half) of a woman's cycle. It is released by the corpus luteum. The corpus luteum is an endocrine organ that forms from the ovarian follicle once an egg has been released.
If ovulation occurs, the corpus luteum begins to create progesterone which peak at around day 21 of the menstrual cycle. It then gradually decreases to baseline levels by the end of the cycle (when the next period begins).
Progesterone helps prepare the uterus and breasts for pregnancy, it also influences moods, appetite and sex drive.
What is Estrogen Dominance?
'Estrogen dominance' is a an umbrella term to denote an increased ratio of estrogen to progesterone hormones that is found in a number of conditions.
Estrogen is ordinarily the dominant hormone during the follicular phase in order to ripen a follicle and trigger ovulation. If ovulation does not occur or the corpus luteum does not function adequately, there is a low amount of progesterone produced during the luteal phase, meaning the estrogen during this phase is relatively higher.
'Estrogen dominance' or a higher estrogen to progesterone ratio, is not a medical diagnosis in and of itself, but is part of a physiological process of some conditions such as endometriosis and adenomyosis, perimenopause, anovulation and luteal phase deficiency.
What Are Estrogen Dominance Symptoms?
The most common signs of estrogen dominance are:
irregular or heavy periods,
premenstrual spotting or spotting through the cycle
feeling bloated,
headaches
breast tenderness
weight gain (especially around the hips and waist),
Estrogen Metabolism
All sex steroids are made from cholesterol through a series of enzyme conversions.
2 important enzymes include StAR and aromatase.
Steroidogenic acute regulatory protein (StAR) brings cholesterol to where it needs to be in the cell for conversion into a sex steroid.
Estradiol, the main estrogen found in females is converted from testosterone to estradiol by an enzyme called aromatase. Another estrogen, Estrone is converted from androstenedione to estrone via aromatase.
Estrogens are metabolised by conversion to inactive metabolites in the liver and excreted via bile into the gut and via the kidney into the urine.
Do I have too much estrogen or is it low progesterone levels?
Rather than focus on estrogen dominance it may be more useful to think about the progesterone levels. Progesterone is typically measured at it's peak, around 7 days prior to when the next period is due to start. This is day 21 if your cycle is 28 days.
If you have a low progesterone rise, you may have ovulated but the corpus luteum makes low progesterone levels this cycle.
If you have no progesterone rise: you did not ovulate this cycle.
Progesterone resistance: In some conditions circulating hormone levels are normal through the cycle, but on a local level cells are more responsive to estrogen and more resistant to progesterone. This means these cells have less progesterone receptors and respond less to progesterone signals. This is seen in endometriosis.
What conditions are associated with 'estrogen dominance' aka relatively low progesterone levels?
'Estrogen dominance' is associated with a number of conditions, such as endometriosis and adenomyosis, perimenopause, anovulation and luteal phase deficiency.
Endometriosis and Adenomyosis
Endometriosis is a condition where the endometrial tissue that normally lines the uterus grows outside of it, usually in the pelvic cavity.
Endometrial cells can be found on the ovaries, fallopian tubes and other structures. This growth is associated with inflammation and can cause pain and infertility.
In endometriosis and adenomyosis there is estrogen dysregulation. This means production of estrogen is not regulated in ordinary ways.
There are at least 4 ways that estrogen production is dysregulated, with the net effect of too much estrogen.
Increased local production of estrogen in the pelvis by up regulation of aromatase enzyme and steroidogenic acute regulatory protein (StAR) activity.
The estrobolome is the collection of genes in the gut microbiome that are involved in regulating estrogen metabolism. These genes regulate the amount of excess estrogen that is expelled or reabsobed into the body. When this activity is impaired due to a dysbiotic (imbalanced) gut microbiome, excess estrogen is retained in the body. (Int J Mol Sci. 2021)
The gut metabolome is the sum of metabolites from the gut. There is a two-way connection between the but and the brain called the Gut-brain-axis. Active metabolites made in the gut communicate with the brain, bind to GnRH receptors and stimulate LH and FSH which stimulate estrogen production.
The endometrial lesions in the pelvis express more estrogen receptors than endometrium in the uterus, increasing the effects of estrogen in those cells (Iran J Reprod Med. 2015).
Fibroids
Fibroids are non-cancerous growths that can occur in the uterus. They are made up of smooth muscle cells and collagen fibres.
Fibroids overexpress aromatase and 17β-HSD enzymes which increase estradiol levels.
One of the major roles of estrogen in fibroid development appears by increasing the production progesterone receptors as well as growth factors such as IGF-1.
Research indicates that it is this increased estrogen that provokes higher progesterone receptor stimulation as well as growth factors that produces fibroid growth (Reprod Sci 2017).
Luteal phase deficiency
Luteal phase deficiency is where there is a low progesterone level in the luteal phase of the menstrual cycle.
With luteal phase deficiency there is insufficient progesterone exposure to maintain a normal secretory endometrium and allow for normal embryo implantation and growth, so it can impact fertility (Obstet Gynecol Clin North Am. 2015).
It is considered under the umbrella of estrogen dominance not because there are high levels of estrogen in the body, but because the levels or progesterone are low in relation to the estrogen during the luteal phase.
It can occur at any age, occur in 4-8 percent of cycles in women with regular cycles. It is most common during perimenopause when women are transitioning out of their reproductive years.
LPD is sometimes can manifests in a number of ways.
as a shortened luteal phase lasting less than 9 days, from ovulation to menstrual bleeding.
pre-menstrual spotting that begins days before menstruation.
irregular periods
recurrent pregnancy loss
difficulty conceiving
Other medical conditions affecting the thyroid or the pituitary can cause luteal phase deficiency so these should be excluded.
Luteal phase deficiency can also occur in PCOS.
Anovulatory cycles
Anovulatory cycles are menstrual cycles without ovulation.
It can occur in women of any age. It can be caused by hormonal imbalances, reduced energy intake, stress, thyroid problems or PCOS.
During anovulatory cycles there is still estrogen production but not enough to ripen a follicle for egg release at ovulation.
Anovulatory cycles can occur in PCOS.

During anovulatory cycles the estrogen levels are not high enough during the follicular phase to ripen a follicle and create a mid-cycle surge of estrogen.

The lack of a mid-cycle surge of estrogen means no ovulation, no formation of the corpus luteum from the follicle and no progesterone rise, so the net effect is a higher than normal estrogen to progesterone ratio.
Perimenopause
Perimenopause is the phase during which women transition out of their reproductive years both luteal phase deficiency and anovulatory cycles become increasingly common in this age group.
Progesterone levels are the first to decline, causing issues like more irregular periods, heavier periods, premenstrual spotting, premenstrual headaches and due to the higher unopposed estrogen levels this also contributes to insulin resistance, and storage of energy as visceral fat (or fat around the tummy area) and weight gain.
Learn about the Symptoms of perimenopause, the 5 lifestyle pillars of perimenopause health, and NZ Hormone Replacement Therapy (HRT) options.
Is breast cancer caused by 'estrogen dominance'?
Estrogen is required for normal breast development and is found in normal breast cells.
Cancer initiation is a complex interplay between genes, inflammation, the immune system, cellular metabolism, lifetime exposure to environmental toxins and hormones.
Estrogen is used by most cells in the body including the brain, muscles, bones, breast, uterus, gut, and bladder cells. In some people, estrogen in combination with other factors seems to play a in protecting against breast cancer.
The Women's Health Initiative is a long clinical trial that looked at post-menopausal women who were given oral estrogen hormone replacement therapy (HRT) alone or oral estrogen with a synthetic progestogen. It demonstrated over 20.3 years of follow-up that use of oral estrogen therapy alone (without the use of a synthetic progestogen) was associated with a reduced 26% breast cancer risk and 40% reduced death from breast cancer. This was compared with women who did not use any hormone replacement therapy. (JAMA 2020)
Breast cancer risk is slightly increased in both the use of the combined oral contraceptive pill and progestogen only contraception (PLOS 2023). This increased risk is attributed to the use of synthetic progestins rather than estrogen.
Breast cancer risk and estrogen exposure is related to lifetime estrogen exposure so women who have earlier periods, are older at first pregnancy, have fewer pregnancies and who breast feed for shorter times have lifetime exposure to their own exogenous hormones that is less protective against breast cancer.
Are hormone tests useful for 'estrogen dominance' associated conditions?
Hormone testing can be a useful tool for understanding and managing some forms of estrogen dominance aka: anovulation, luteal phase deficiency. This most commonly occurs in the fertility setting.
It is also important to check thyroid hormones, testosterone levels and prolactin if periods are irregular to see if thyroid, pituitary issues are present or if you have polycystic ovarian syndrome.
Hormone testing is not useful for endometriosis, adenomyosis, fibroids as higher estrogen if found produced locally by the lesions themselves not by the ovaries.
It is important to remember that hormone levels change from hour to hour and day to day and that one cycle can be anovulatory, the next ovulatory with a luteal phase deficiency and another ovulatory with normal luteal phase. The female body and their hormonal systems are very dynamic and responsive to diet, stress, exercise and other external inputs that influence the immune-gut-brain-ovary axis.
What do hormone tests show?
Standard medical testing of hormones looks at hormones in 2 phases of the menstrual cycle.
Follicular Phase Hormone Testing
This is done on day 2-3 of the cycle. Estrogen hormone testing checks your estrogen levels when they are at their lowest. This gives us an indication of your baseline estrogen levels during this cycle.
We can also check follicle-stimulating hormone and luteinizing hormone. The FSH/estradiol ratio can indicate adequate signalling between the pituitary and the ovaries for an ovulatory cycle.
If LH and FSH are too high they can indicate post-menopause.
If LH, FSH and estradiol are low they can indicate functional amenorrhea or Relative energy deficiency in sports (RED-S) or lactational amenorrhoea.
Luteal Phase Hormone Testing
During the follicular phase we want to see if you have ovulated or made sufficient progesterone.
Progesterone levels taken approximately 7 days prior to the end of your cycle.
Any testing done is best combined with cycle tracking, and natural fertility monitoring which involves early morning temperature and cervical mucous tracking.
Some women also combine this cycle testing with luteinizing hormone testing around day 14 of the cycle to check for ovulation especially if investigating infertility.
Some women have also started using home testing devices such as Mira which check hormone metabolites and can be helpful monitor hormones across the menstrual cycle to determine if anovulation or luteal phase deficiency is present.
The Takeaways
"Estrogen dominance" is an umbrella term used to describe conditions where either during the luteal phase of the cycle or in the local tissues (such as endometrial lesions and fibroids) there is a higher estrogen to progesterone ratio.
Estrogen dominance can look like an anovulatory cycle, luteal phase deficiency, and is present in many conditions including PCOS, endometriosis, adenomyosis, fibroids,
Estrogen dominance does not cause cancer but increased estrogen exposure over a lifetime, combined with other complex gene, biological and environmental factors can increase the risk of breast cancer.
Hormone testing during your cycle can be useful depending on what the cause of estrogen dominance you are experiencing.
Where can I get started?
Tracking and getting to know your cycle and symptom patterns is a great place to start.
If you need additional medical advice, Dr Deb Brunt @ Ōtepoti Integrative Health would love to support you with your period and menstrual health whether it be irregular, painful or heavy periods and no matter what stage of life from puberty to perimenopause.
She practices holistic medicine in New Zealand and Menopause health coaching internationally. She has a passion for supporting women adapt to their changing female physiology for optimum health and wellbeing.
Dr Deb Brunt | Ōtepoti Integrative Health | Book Appointment
References
Chlebowski RT, Anderson GL, Aragaki AK, et al. Association of menopausal hormone therapy with breast cancer incidence and mortality during long-term follow-up of the Women’s Health Initiative randomized clinical trials. JAMA. 2020;324(4):369-380.
Fitzpatrick D, Pirie K, Reeves G et al. (2023) Combined and progestagen-only hormonal contraceptives and breast cancer risk: A UK nested case–control study and meta-analysis. PLoS Med 20(3): e1004188.
Jiang I, Yong PJ, Allaire C, et al. Intricate Connections between the Microbiota and Endometriosis. Int J Mol Sci. 2021 May 26;22(11):5644.
Garavaglia E, Audrey S, Annalisa I, et al. Adenomyosis and its impact on women fertility. Iran J Reprod Med. 2015 Jun;13(6):327-36.
Borahay MA, Asoglu MR, Mas A, et al. Estrogen Receptors and Signaling in Fibroids: Role in Pathobiology and Therapeutic Implications. Reprod Sci. 2017 Sep;24(9):1235-1244.
Mesen TB, Young SL. Progesterone and the luteal phase: a requisite to reproduction. Obstet Gynecol Clin North Am. 2015;42(1):135-151. doi:10.1016/j.ogc.2014.10.003
Wen C, Wu L, Fu L, et al. Unifying mechanism in the initiation of breast cancer by metabolism of estrogen (Review). Mol Med Rep. 2017 Aug;16(2):1001-1006.
.png)
Comments